Going to therapy can be a big step for anyone, including first responders. Because of the unique challenges that come with emergency service work – such as exposure to trauma, violence, and high-pressure situations – therapy often needs to be tailored specifically to their experiences.
First session
- Initial assessment: The first 1–2 sessions usually focus on understanding the individual’s background, job role (e.g., firefighter, police officer, paramedic, volunteer), trauma history, current mental health, and goals. Therapists may use structured interviews or screening tools such as PTSD checklists or depression/anxiety scales to guide this process.
- Building trust and safety: Many first responders are hesitant to open up due to stigma, concerns about judgment, or worries about career impact. A strong therapeutic relationship is crucial, and therapists work to create a safe, respectful, and non-judgmental environment.
- Confidentiality explained: Clinicians will outline the limits of confidentiality which apply to all psychologists, social workers, and counsellors in Australia. These include the steps taken if someone is at risk of harming themselves or others. Understanding how personal health information is collected and stored is also an important part of this discussion.
Future sessions
Therapy sessions, which are usually 50 minutes, often begin with a brief check-in about recent life events or crises before returning to the individual’s broader goals. Different evidence-based approaches may be used, such as:
- Cognitive Behavioural Therapy (CBT): Reframes negative thoughts and builds coping strategies; commonly used for anxiety, depression, and PTSD.
- Eye Movement Desensitisation and Reprocessing (EMDR): Helps process traumatic memories, often for PTSD.
- Exposure Therapy: Gradual, safe exposure to trauma reminders to reduce avoidance and fear.
- Mindfulness and stress reduction: Breathing, grounding, and relaxation techniques to calm the body’s stress response.
Therapy may also incorporate:
- Education and skill building: Learning about stress responses and resilience, and developing tools such as emotional regulation, communication, and self-care.
- Relationships and communication: Exploring family, peer, or team dynamics; sometimes involving family members or referring to peer support or couples’ therapy.
- Self-identity and values: Addressing moral injury, disillusionment, or identity concerns – particularly for those approaching retirement or transitioning roles. Therapy can help reconnect first responders with their values, purpose, and self-esteem.
The process of change
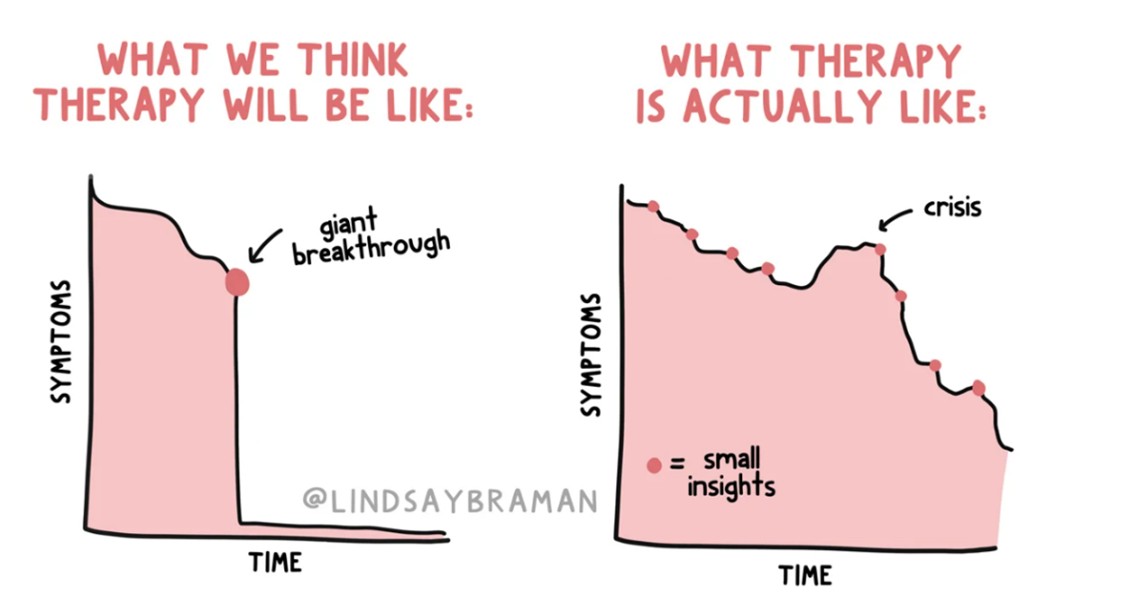
It’s important to understand that therapy is rarely a straight path from feeling unwell to feeling better. Progress can include ups and downs—some insights and breakthroughs, some symptom improvement, and sometimes periods where symptoms feel worse before they improve. Change often happens gradually, through small shifts in thoughts, feelings, and behaviours that build toward better overall wellbeing, as outlined in this illustration by @lindsaybraman.
Final thoughts
Starting therapy can feel daunting, but with the right support and realistic expectations, it can be an enormously beneficial step toward recovery, resilience, and renewed purpose.
Kim Harrison
Senior Psychologist, Clinical Content Creator and Facilitator
Fortem Australia
Kim is a clinical psychology registrar with a background in organisational psychology and experience working with police members. She is passionate about mental health literacy and aims to translate up-to-date psychological research into easily understood information.
